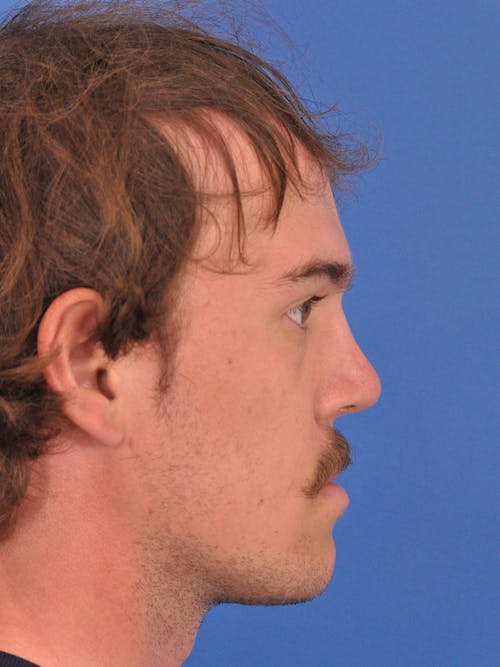
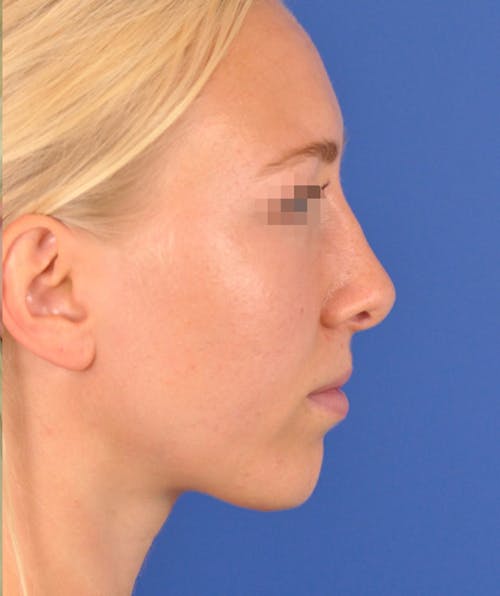
Enhance your facial harmony and confidence with expert rhinoplasty at Guelph Facial Plastics. Dr. Brace, a double board-certified facial plastic surgeon, specializes in precision nose reshaping to achieve natural-looking, balanced results. We proudly serve patients from Guelph and the surrounding Ontario areas of London, Kitchener, and Milton.
Who is a Candidate for Rhinoplasty?
The nose plays both a central aesthetic role in facial beauty and a functional role in breathing. You may be considering a rhinoplasty if you feel the shape, size, or symmetry of your nose distracts from the overall aesthetic balance and harmony of your face. If you also have difficulties with nasal breathing, altering the shape of the nose will often also improve nasal airflow and breathing. In some cases, the septum (the middle wall on the inside of the nose) is also reshaped and straightened in which case the surgery is referred to as a ‘septorhinoplasty’.
Men and women of every ethnicity and background pursue rhinoplasty for a variety of reasons. Age plays a factor and, in general, a young adult should be finished growing before pursuing surgery. There are familial, cultural, and ethnic considerations for every person and every nose. Techniques vary for each type of nose. A consultation to determine your personal aesthetic goals and an exam of your nose is required to create an individual and specific surgical plan.